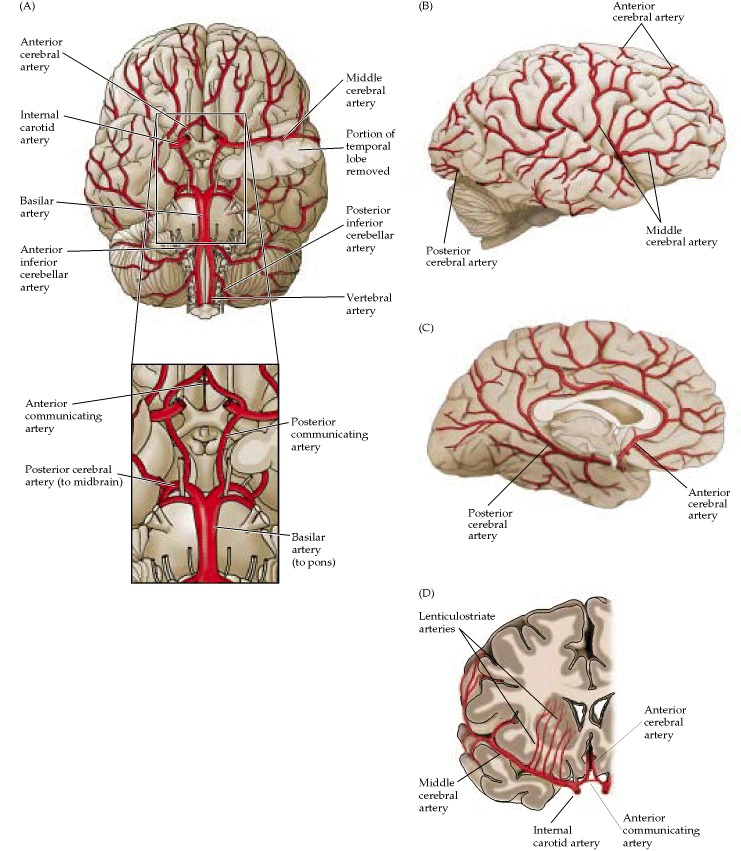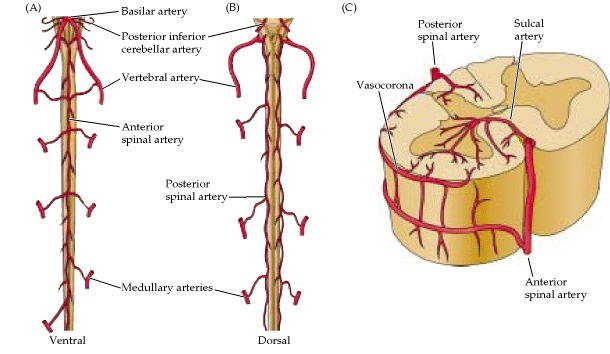
Multiple sclerosis (MS) is an inflammatory autoimmune disease in which myelin sheaths around nerve cells of the brain and spinal cord are damaged, leading to loss of myelin and scarring. When this nerve covering is damaged, nerve signals slow down or stop. The nerve damage is caused by inflammation. Inflammation occurs when the body's own immune cells attack the nervous system. This can occur along any area of the brain, optic nerve, and spinal cord.
MS affects women more than men. The disorder is most commonly diagnosed between ages 20 and 40, but can be seen at any age. It is unknown what exactly causes this to happen. The most common thought is that a virus or gene defect, or both, are to blame. Environmental factors may play a role. You are slightly more likely to get this condition if you have a family history of MS or live in an part of the world where MS is more common.
Symptoms
Symptoms vary, because the location and severity of each attack can be different. Episodes can last for days, weeks, or months. These episodes alternate with periods of reduced or no symptoms (remissions). Fever, hot baths, sun exposure, and stress can trigger or worsen attacks. Heat intolerance in MS shows up as a "pseudoexacerbation" - the experience of having symptoms appear or worsen due to heat exposure. This is different than a true relapse. In the case of a pseudoexacerbation, when the body’s temperature returns to normal, these symptoms disappear. No damage, such as inflammation, demyelination or new lesions, has been done during these pseudoexacerbations.
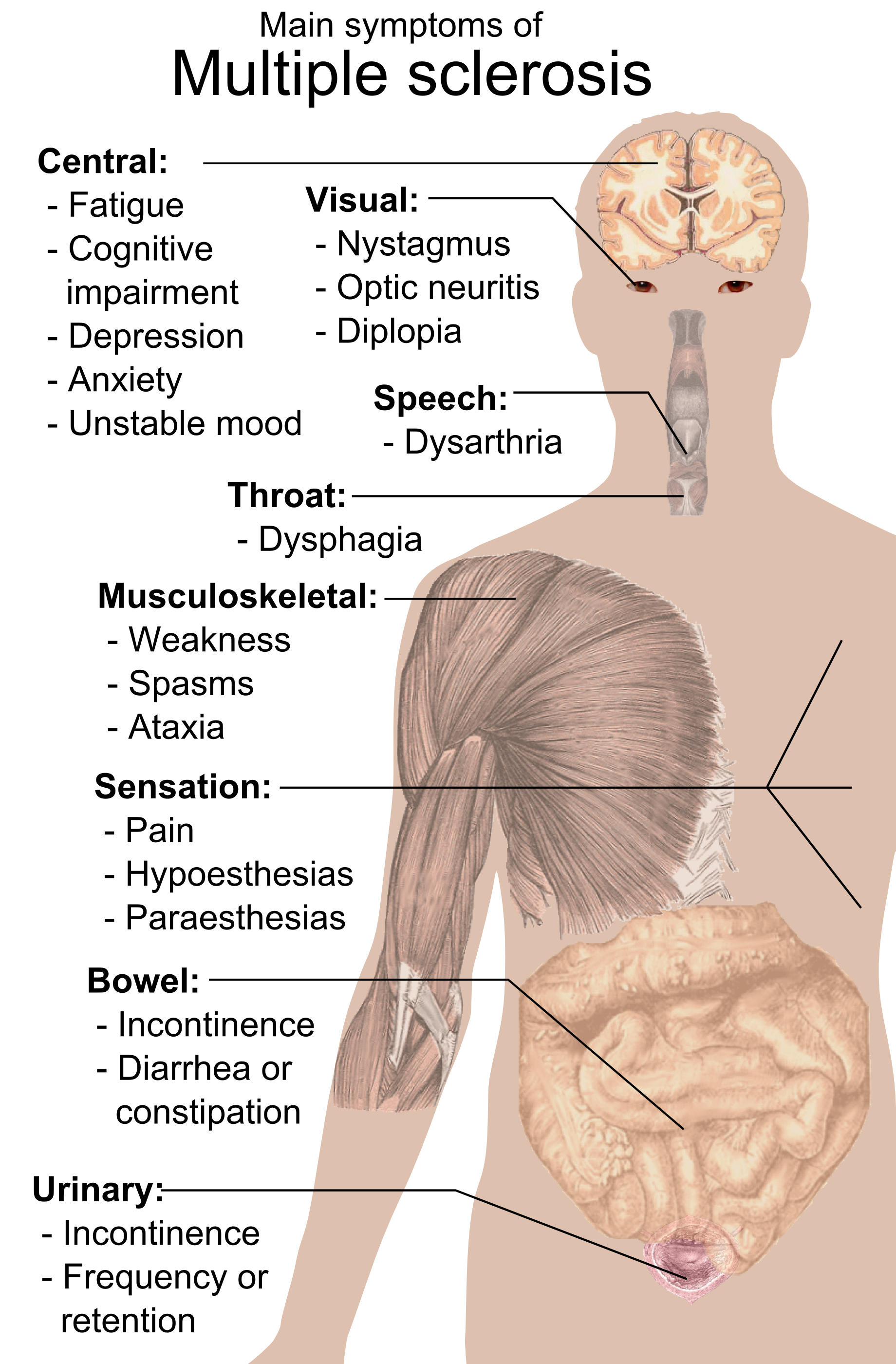
It is common for the disease to return (relapse). However, the disease may continue to get worse without periods of remission. Because nerves in any part of the brain or spinal cord may be damaged, patients with multiple sclerosis can have symptoms in many parts of the body - see the picture above for the main symptoms.
How does heat affect MS?
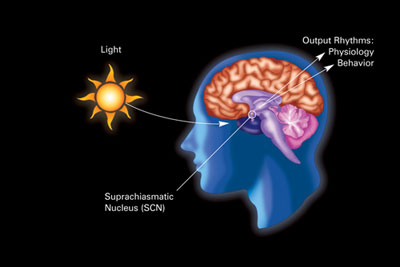
Demyelination slows the ability of the nerves to function, and heat further slows down nerve impulse transmission in demylinated regions. Even a very slight increase of as little as one-quarter to one-half a degree in the body’s core temperature is enough to cause symptoms of heat intolerance.
Multiple sclerosis is a demyelinating disease of the central nervous system, characterized by a relapsing and remitting or, alternatively, by a steady and continuous course of dysfunction. The hallmark of the disease is heterogeneity. How the disease presents itself depends on the exact location and total accumulation of lesions and on the impact of demyelination on nerve conduction. Conduction maybe be enhanced, producing positive symptoms like tic douloureux, paresthesia, or tingling, or conduction may be diminished, producing negative symptoms like blindness and paralysis. Diminished conduction may be total or partial, with decreases in the maximum of frequency or velocity of conduction. During remission, which may last months or years, symptoms improve as inflammation subsides, sodium channels migrate into the bare axon, remyelination of the denuded site occurs, and, ultimately, conduction resumes through the lesion sites. The deficit may also become permanent as axons degenerate. During shorter periods lasting hours or days, symptoms may also worsen, as conduction through old lesions fluctuates; conduction is “highly insecure” and subject to inflammatory factors like nitric oxide and temperature changes.
Heat worsens and cooling improves negative symptoms of multiple sclerosis, sometimes dramatically so. The underlying mechanism relates to the influence of temperature on sodium channels and on current necessary for depolarization of the axon. Increases in temperature diminish the depolarizing current, whereas decreases in temperature have the opposite effect. Sensitivity can be extreme, and very small changes can have profound effects. Heating, for example by radiation from the sun, can turn a limping gait into no gait at all. Alternatively, hot air from a hair dryer can turn a hopeful morning into an exhausting one. Cooling, on the other hand, by sitting in a cool bath or shower, can turn the “disease off” (at least for a little while) and give an individual back the freedom for exercise or work.
A University of Michigan researcher, Dr. Joseph Cannon, studied the effects of exercise on the immune system in rats and humans. He noted that the immune system may become more active in any situation when there’s a rise in body temperature (such as during strenuous activity); in other words, that exercise can have the same effect on the immune system as fever does. Since the immune system takes its cue from a rise in body temperature during illness, it evidently does the same when any rise in temperature occurs, such as during strenuous exercise, a hot day, a hot bath, or emotional stress.
Any increase in temperature, then, could result in a situation where white blood cells may be produced to fight an enemy—with no enemies around to fight! Imagine some of these white blood cells entering the CNS, gathering at various points along the nerves. These gatherings of white blood cells result in inflammation, or swelling, resulting in pressure, or a “squeeze” on nerve cells in the area. Depending on which nerve cells are being squeezed, new symptoms may appear in that part of the body associated with those nerve cells.
Diagnosis
Symptoms of MS may mimic those of many other nervous system disorders. The disease is diagnosed by ruling out other conditions. People who have a form of MS called relapsing-remitting may have a history of at least two attacks, separated by a period of reduced or no symptoms.
The health care provider may suspect MS if there are decreases in the function of two different parts of the central nervous system (such as abnormal reflexes) at two different times.
A neurological exam may show reduced nerve function in one area of the body, or spread over many parts of the body. This may include:
- Abnormal nerve reflexes
- Decreased ability to move a part of the body
- Decreased or abnormal sensation
- Other loss of nervous system functions
An eye examination may show:
- Abnormal pupil responses
- Changes in the visual fields or eye movements
- Decreased visual acuity
- Problems with the inside parts of the eye
- Rapid eye movements triggered when the eye moves
Tests to diagnose multiple sclerosis include:
- Lumbar puncture (spinal tap) for cerebrospinal fluid tests, including CSF oligoclonal banding
- MRI scan of the brain and MRI scan of the spine are important to help diagnose and follow MS
- Nerve function study (evoked potential test)
Treatment
There is no known cure for multiple sclerosis at this time. However, there are therapies that may:
- slow the disease through medication
- treat exacerbations (also called attacks, relapses, or flare-ups) by reducing inflammation through corticosteroids
- manage symptoms
- improve function and safety through physical therapy
- provide emotional support
Are there alternative therapies for MS?
Complementary and alternative medicine (CAM) includes a variety of interventions - from exercise and dietary supplements to stress management strategies, biofeedback, and acupuncture. These therapies - which come from many different disciplines and traditions - are generally considered to be outside the realm of conventional medicine. When used in combination with conventional medicine, they are referred to as “complementary;” when used instead of conventional medicine, they are referred to as “alternative.” In the United States today, approximately 75% of people with MS use one form or another of CAM, generally in combination with their prescribed MS treatments.
Physical Therapy and MS
The role of rahabilitation in managing MS:
- Physical therapy, speech therapy, occupational therapy, and support groups
- Assistive devices, such as wheelchairs, bed lifts, shower chairs, walkers, and wall bars
- A planned exercise program early in the course of the disorder
- A healthy lifestyle, with good nutrition and enough rest and relaxation
- Avoiding fatigue, stress, temperature extremes, and illness
- Changes in what you eat or drink if there are swallowing problems
- Making changes around the home to prevent falls
- Social workers or other counseling services to help you cope with the disorder and get assistance (such as Meals-on-Wheels)
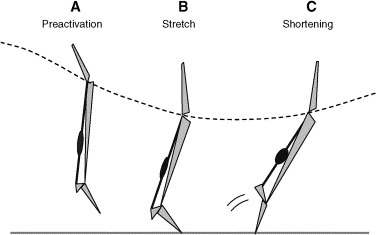
Physical Therapy cannot treat the primary symptoms of MS, but can do a lot of things for the secondary effects that are the result of them. The Physical Therapist evaluates and addresses the body’s ability to move and function, with particular emphasis on walking, strength, balance, posture, fatigue, and pain. PT might include stretching, range-of-motion and strengthening exercises, gait training, and training in the use of mobility aids (canes, crutches, scooters and wheelchairs) and other assistive devices.
The ultimate goal is to achieve and maintain optimal functioning and prevent unnecessary complications such as de-conditioning, muscle weakness from lack of mobility, and muscle contractures related to spasticity. Building a treatment plan, a Physical Therapist should follow the WHO's ICF model and base his strategy based on that. I have already posted an article about a beautiful tool one can use in order to build his strategy - the getptsmart.com. Regarding body structures and functions, a Physical Therapist should evaluate and manage:
The ultimate goal is to achieve and maintain optimal functioning and prevent unnecessary complications such as de-conditioning, muscle weakness from lack of mobility, and muscle contractures related to spasticity. Building a treatment plan, a Physical Therapist should follow the WHO's ICF model and base his strategy based on that. I have already posted an article about a beautiful tool one can use in order to build his strategy - the getptsmart.com. Regarding body structures and functions, a Physical Therapist should evaluate and manage:
- Pain
- Fatigue and fitness level
- Balance problems and poor coordination
- Muscle strength
- Bladder and bowel control
Taking into consideration the personal and environmental factors of the specific patient together with the specific activities and participation limitations will help the Physical Therapist build a successful program tailored to the patient he is dealing with. Patient and family education always plays a major role in the rehabilitation process.
Some general techniques used in Physical Therapy are the following:
- Stretches to prevent or ease spastic muscles
- Moves to keep muscles strong
- Range-of-motion exercises
- Gait training for easier walking
- Learn to use canes, crutches, scooters, wheelchairs, or other aid
Furthermore, taking advantage of the cooling properties of water may help attenuate the consequences of heat sensitivity. In a study done by White et al. (2000), exercise pre-cooling via lower body immersion in water of 16-17°C for 30 minutes allowed heat sensitive individuals with MS to exercise in greater comfort and with fewer side effects by minimizing body temperature increases during exercise. Hydrotherapy exercise in moderately cool water of 27-29°C water can also be advantageous to individuals with MS. Temperatures lower than 27°C are not recommended because of the increased risk of invoking spasticity.
Here is a a Physical Therapy case study that uses the getptsmart.com tool. I find it amazing.
Sources: